25 Feb Japanese Encephalitis Virus vaccine was running low, here is what you need to know
Japanese Encephalitis Virus (JEV) is relatively unknown, even though it has been the leading cause of viral encephalitis in Asia for the last 20 years. The disease is a mosquito-borne viral infection, which has spread from East Asia to the Oceania region in the last two decades and could spread further into mainland Australia in the coming years.
There were false reports that vaccines for JEV were in short supply, which raised concerns, especially in the Philippines. This then lead to an actual shortage of supply of the vaccine. Suppliers of the vaccine quickly attempted to reassure people that there was no shortage, but it was too late. The concern had already led to increases in demand for the vaccine compared with usual usage. Resulting in the lack of readily available vaccines in the Asian region. Suppliers then amended this shortage by increasing shipments of the vaccine to all affected areas, resolving these issues.
Families in high endemic regions have expressed their concerns that vaccines are overpriced as the vaccine costs more than average wages per month. Consequentially, parents are deciding not to get children vaccinated against the disease. This could result in an outbreak in the future. Currently, suppliers are investigating whether they can reduce manufacturing price so that it will help ease the reported overpricing.
To help with these issues, the Department of Health in various Asian regions are currently working on including the JEV vaccine in national immunisation programmes for 2018. Currently 50% of the Asia and West Pacific region have national immunisation programmes in place for the JEV vaccine. Having national immunisation programmes makes the vaccine more readily available and free.
In other countries such as the UK, vaccines are recommended for people who are travelling to high risk areas. However, this vaccine is not free on the NHS, so people will have to pay for it themselves. The cost for this vaccine in the UK is around £90, which is quite expensive, and people tend not to factor this in when budgeting for trips to high endemic regions.
After the reports on availability and cost of vaccines, it highlights the importance to learn key information about the disease. This blog answers 7 key questions about the disease which will provide you with the essential information. The answers to the questions are vital for people who are at high risk of the disease whether they are travelling, living or working in close vicinity to the pathogen.
1) What is Japanese Encephalitis virus?
JEV was first documented back in 1871 in Japan. Similarly, to dengue, yellow fever and West Nile viruses, JEV is an example of a flavivirus. Flaviviruses are all classified as arboviruses due to their mechanism of transmission through an infected arthropod, in this case a mosquito. JEV causes encephalitis, which is the inflammation of the brain caused by an invading infection that directly invades the brain.
2) How is JEV transmitted?
JEV is transmitted through arthropod, specifically the mosquito species: Culex tritaeniorhynchus which is the vector for the disease. The virus exists in a transmission cycle between mosquitos, pigs and water birds, meaning the pathogen has a transmission cycle known as an enzootic cycle. In an enzootic cycle, pigs and aquatic birds serve as amplification and reservoir hosts, providing the source of infection for the mosquito vectors. Humans are the end users and cannot transmit the disease. Mosquitos are mainly found in rural areas, suburbs and commuter towns making these highly endemic regions.
3) Who are at risk of JEV?
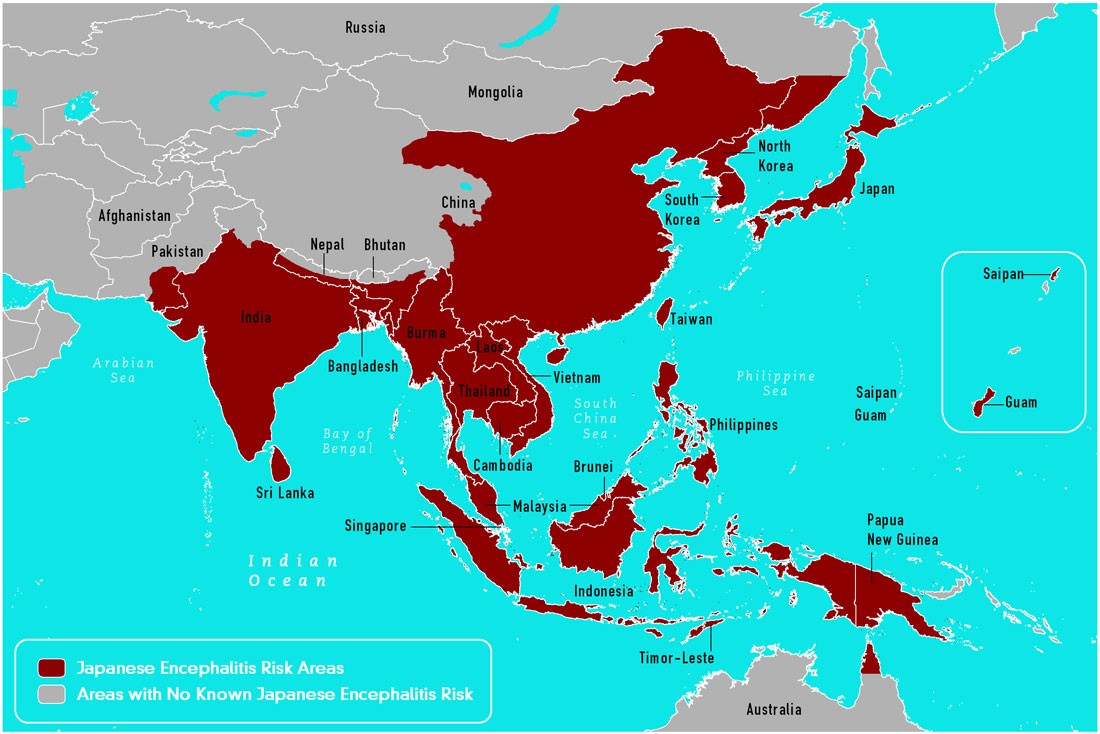
Currently, those who live or have travelled to JEV-endemic regions are at the highest risk of catching the disease. JEV is the leading cause of vaccine preventable encephalitis in Asia and the Western Pacific and accounts for an estimated 68,000 clinical cases per year. Of these, up to 20,000 cases result in death. JEV primarily affects children, with adults developing immunity after being infected as a child. It is possible that individuals of any age can be affected. This figure below displays the countries that are at high risk of the disease.
4) When can JEV be transmitted?
JEV seems to be mostly transmitted during the warm season, which can cause large epidemics. In highly tropical regions, the transmission can be high all year round with more than 3 billion people at risk of the infection. The JEV transmission can also intensify over rainy seasons as the vector population increases. Within high endemic regions, 1 in 10 people can be infected with the disease during outbreaks.
5) How serious is JEV?
JEV can be very serious. Most JEV infections are mild, but 1 in 20 cases develop into encephalitis, resulting in severe clinical illnesses. The fatalities caused by the pathogen can be as high as 30% emphasising the severity of the disease. Of those who do survive, 20%-30% suffer permanent intellectual, behavioural and neurological problems. The extent of the permanent damage varies, but problems such as paralysis, recurrent seizures or the inability to talk are common.
6) Is JEV preventable?
There is a well performing vaccine that is more than 90% effective and is available to prevent the disease. Since the 1930’s, different vaccines have been used, but the most popular and cost effective is the live attenuated SA14-14-2 vaccine that was developed in 1988. As well as being given a vaccine, those who visit countries with high levels of JEV are advised to avoid mosquito bites as much as possible. This could be through personal preventative measures such as repellents and wearing suitable clothing. Currently there is no direct treatment for patients infected with JEV, so it is imperative to use vaccines or methods of mosquito bite avoidance. Even with the preventative measures, major outbreaks occur every few years.
7) How to test for JEV?
To confirm the diagnosis of JEV, an IgM antibody-capture enzyme linked immunosorbent assay (MAC-ELISA) is the current standard method. It should be noted that this method only detects 90% of cases and efficacy is further compromised when JEV is in co-circulation with other flaviviruses, which can often be the case. As most flaviviruses cause higher expression levels of IgM, the MAC-ELISA method cannot distinguish whether the higher level of IgM is due to JEV infection or to an infection caused by the other co-circulating flavivirus.
The new molecular approach of qPCR for nucleic acid detection is revolutionising the field of JEV diagnostics, as the high specificity of this method distinguishes between the different flaviviruses. The advantage of qPCR is that the test is rapid, sensitive and highly specific to the target RNA sequence uniquely found only in JEV.
Primerdesign produces the genesig Real-Time PCR Kit for JEV which directly tests for the JEV pathogen with sensitivity to less than 100 copies of target. The kit can be run on all qPCR cyclers as well as the genesig q16, the most affordable qPCR instrument on the market. The primers have 100% homology and were designed for the detection of all 5 genotype variations of JEV. Click here for more information on the kit.
genesig kits are sold for research use only and are not licensed for diagnostic procedures.
References
Barthold, S., Dubovi, E., Maclachlan, J., Swayne, D., Winton, J. (2016) Fenner’s Veterinary Virology [Fifth Edition]. Elsevier Inc
Castillo, J. (2017) Japanese Encephalitis: Doctors discuss vaccine shortage and price. [Online]
Centres for disease control and prevention (2015) Japanese encephalitis fact sheet [Online]
Han, N., Adams, J., Chen, P., Guo, Z., Zhong, X., Fang, W., Li, N., Wen, L., Tao, X., Yuan, Z., Rayner, S. (2014) Comparison of genotypes I and III in Japanese encephalitis virus reveals distinct differences in their genetic and host diversity. Journal of Virology. 88(19) pp 11469-11479
Heffelfinger, J., Batmunkh, N., Grabovac, V., Diorditsa, S., Liyanage, J., Pattamadilok, S., Bahl, S., Vannice, K., Hyde, T., Chu, S., Fox, K., Hills, S., Marfin, A. (2017) Japanese Encephalitis surveillance and immunization- Asia and Western pacific regions, 2016. Weekly Morbidity and Mortality Weekly Report. 66(22)., 579-583
Johnson, B., Goodman, C., Jee, Y., Featherstone, D. (2016) Differential diagnosis of Japanese encephalitis virus infections with the Inbios JE detect and DEN detect MAC-ELISA kits. The American Journal of Tropical Medicine And Hygiene. 94(4) pp 820-828
Liu, D. (2016) Molecular detection of human viral pathogens. CRC Press., pp 181-208
Mackenzie, J., Gubler, D., Peterson, L. (2004) Emerging flavivirus: the spread and resurgence of Japanese encephalitis, West Nile and dengue viruses. Nature Medicine. 10 pp 98-109
Mansfield, K., Horton, D., Johnson, N., Li, L., Barrett, A., Smith, D., Galbraith, S., Solomon, T., Fooks, A. (2011) Flavivirus induced antibody cross reactivity. Journal of General Virology. 92(12) pp 2821-2829
Shirato, K., Miyoshi, H., Kariwa, H., Takashima, I. (2005) Detection of West Nile virus and Japanese encephalitis virus using real-time PCR with a probe common to both viruses. Journal of Virological Methods. 126(1) pp 119-125
Solomon, T., Dung, N., Kneen, R., Gainsborough, M., Vaughn, D., Khanh, V. (2000) Japanese encephalitis. Neurological Aspects of Tropical Disease. 68 pp 405-415
Swami, R., Ratho, R., Mishra, B., Singh, M. (2008) Usefulness of RT-PCR for the diagnosis of Japanese encephalitis in clinical samples. Scandinavian Journal of Infectious Diseases. 40(10) pp 815-820
Toriniwa, H., Komiya, T. (2006) Rapid detection and quantification of Japanese encephalitis virus by real-time reverse transcription look mediated isothermal amplification. Microbiological Immunology. 50(5) pp 379-387
World Health Organisation (2015) Japanese encephalitis fact sheet [Online]